|
by Dr. S. Dawn Dinger, DVM  In part one of this blog on vaccination, we discussed some general information and answered some frequently asked questions regarding vaccinations. In part II we will discuss the current recommendations for canine vaccinations and what diseases they are protecting against. Core vaccinations are considered vital for all dogs due to how common the disease is, the risk of exposure, the severity, or the potential risk to people. These include the DHPP (we will discuss what this means below) and the rabies vaccinations. There are also several other “non-core” vaccinations as well. These are vaccines that protect again diseases that may be less common in different areas of the country, or may be less of a concern depending on the life style of the pet. These include Leptospirosis, Lyme Disease, Bordetella and Canine Influenza. It is important to note that these diseases do not necessarily cause less severe disease. So what exactly are these diseases and how do they affect our pets?  1) DHPP: the letters of this vaccination stand for the individual diseases that this combination vaccine protects against. D = Distemper: a highly contagious and very serious virus of dogs (and some wildlife) spread by aerosol and direct contact with infected animals or contaminated objects. It can lead to pneumonia, severe vomiting and diarrhea and seizures. It is often fatal and those dogs that do survive may have permanent neurological damage. Vaccination is recommended for all dogs and puppies. H = Infectious Canine Hepatitis: also highly contagious this virus leads to acute liver failure, but can also affect the lungs, GI tract, kidneys and eyes. This infection can be fatal and vaccination is recommended for all dogs and puppies. P = Parvovirus: Highly contagious, this virus is spread from dog to dog by secretions and lasts for at least 6 months in the environment. Signs include severe vomiting, bloody diarrhea, greatly decreased white bloods cells (which fight infection), fever, severe dehydration and sometimes death especially in puppies. Vaccinations is recommended for all dogs and puppies. P = Parainfluenza: part of the “kennel cough” complex, this virus affects the respiratory tract and typically leads to coughing, fever, nasal discharge and lethargy. It is usually included in the “core” vaccinations that all dogs and puppies receive. 2) Rabies: This is a fatal viral infection of all mammals, including humans. It is spread via saliva and attacks the central nervous system leading to behavioral changes and paralysis. There is no treatment once signs develop. Unfortunately, there is also no way to test for rabies on a live animal – if rabies testing is required, for example if an unvaccinated animal bites someone or develops suspicious neurologic signs, this test must be performed on brain tissue. Vaccination is recommended for all dogs and puppies over 12 weeks of age and is typically required by law in most states, including Pennsylvania.  3) Leptospirosis: Caused by a bacterium, this disease leads to fever, lethargy, joint pain and kidney and liver failure. It is also “zoonotic” - meaning people can get this as well. It is spread by direct contact, especially with urine of other dogs and wildlife and is often found in contaminated water and soil. Although not considered a “core” vaccine, leptospirosis vaccination is typically recommended at GVVH due to the high amount of leptospirosis we have in the area and the potential severity to both pets and people. 4) Lyme Disease: A tick-borne disease which can lead to limping, joint pain and kidney disease. In 2015 Pennsylvania had the highest number of confirmed Lyme cases in people in the United States and the 2nd highest in dogs. Due to the high incidence of the disease here, we typically recommend vaccination for dogs and puppies.  4) Bordetella: Part of the “kennel cough” complex, this virus affects the respiratory tract and typically leads to coughing, fever, nasal discharge and lethargy. If your dog has any potential exposure to other dogs, for example at boarding kennels, dog parks, groomers, training classes or dog shows, this vaccination may be recommended. Also note, that many boarding kennels require this vaccination as well. 5) Canine Influenza: A relatively newly recognized disease, the “dog flu” leads to respiratory illness ranging from a mild cough to severe pneumonia. It is highly contagious and is easily spread from dog to dog via aerosol and contaminated objects. The same groups of dogs that are recommended to be vaccinated against Bordetella, will also likely benefit from the Canine Influenza vaccine. Some boarding kennels are beginning to require this vaccination as well.  Rest assured that at their annual wellness appointment, we will review your dog's lifestyle and overall health and make vaccination recommendations tailored to your pet so that he or she will remain healthy and happy members of your family. In the final part of this blog on vaccination we will discuss the diseases and recommended vaccinations for our feline friends. Stay tuned….
8 Comments
by Dr. Kristin K. Burton-Hall, VMD  sIf you have visited GVVH recently you may have been surprised as we offered your pet peanut butter, cheese, canned chicken or canned food. This is part of a new certification we have achieved called Fear Free. Fear Free is an initiative developed by Dr. Marty Becker aimed at using gentle control techniques and calming environments in the veterinary hospital to make veterinary visit easier on the pet and owner. The Fear Free initiative involves much more than simply feeding your pet while he/she is here for an exam. Every member of our staff has completed nine hours of continuing education and training to become certified. Our goal is to make the visit as stress free as possible on your pet. We want them (and you!) to like coming to the veterinarian. Puppyhood and kittenhood are the most crucial times to begin your pet's veterinary health care in a fear free environment. We are striving toward more and more to use food, praise, petting and toys as a distraction from the unpleasant but necessary poking and prodding that we must do to them to keep them healthy. We are also trying to exam your pet in an setting that is less intimidating for him/her. Every pet is an individual and we may need a few tries to learn what works best. For cats this may mean removing the top of the carrier and letting him/her sit in the bottom for most of the exam. Some cats feel safer in a familiar area. For dogs this may mean doing most of the exam with him/her on the floor and only using the exam table briefly to obtain a body weight.  What you can do to help: For cats- Make the carrier a more pleasant place to be. Many owners make the mistake of keeping the carrier hidden away and only bring it out when the cat is going to come to the vet. The cat quickly learns to associate the carrier with a scary car ride and trip to the dreaded vet’s office. Leave the carrier out in your home, occasionally putting food and treats in the carrier as well as a comfortable blanket so that your kitty can go in and out of the carrier as he/she pleases. Practice putting kitty into the carrier closing the door and letting them right back out, then give a tasty treat such as canned food or tuna. This way on the day of your schedule visit it won’t be such a struggle to get your kitty into the carrier. When transporting the carrier do not use the handle. Carry it by the bottom as if you would as fragile gift. Carrying it by the handle, swings kitty causing increased movement and nausea. When placing the carrier in the car, put it on the floor of the backseat, behind the passenger seat, this will also decrease movement of the car moving and keep the car from sliding around on the seat or off the seat. This is the safest place for kitty should you have the extreme misfortune of being involved in an accident with kitty in the car. Keep the carrier covered with a towel and once in the veterinary clinic do not set the carrier of the floor. Cats like to be up high. Being on the floor provides too much frightening stimuli: stamping feet, grabbing hands, and sniffing noses of other pets in the clinic. Bring your kitty while they're hungry. Withhold food for 4-6 hours prior to the appointment. This will make your cat less likely to because nauseated and vomit on the way to the clinic and also make them more interested in any food we may offer during the appointment. Talk with us about any concerns you have; you know your feline friend better than anyone else. There are safe, mild sedatives available to help if you think your pet needs it. For some cats and their owners these are a life saver! For others the stress of trying to give the medication at home before the visit far outweighs any benefits. Some cats may be do worse if food is withheld prior to the appointment. Let us know what you think worked well or didn’t work well at his/her last appointment. The synthetic feline facial pheromone "Feliway" is very calming to some cats but not others. It is available in our clinic via diffuser in our exam rooms. You may also request a towel with Feliway prayed onto it to see if your pet could benefit from pheromones.  For Dogs- Bring your dog hungry. Similarly to our feline friends above, withholding food for 4-6 hours prior to the appointment will make your dog less likely to because nauseated and vomit on the way to the clinic. It can also make them more interested in any food we may offer during the appointment. Dogs tend to eat the tasty treats we offer much better for us than cats do. If your dog is not highly food motivated bringing his/her favorite toy can also be very helpful. We have several dogs who are very happy to hold their ball during their vet visits. Teach your pet to accept handling. This is especially helpful for your puppies. Work with your dog to get them to tolerate you opening his/her mouth, look at his/her ears, play with his/her feet all the while treating and rewarding your pet for tolerating and accepting the handling. There should not be any part of your pet’s body that you can not touch. This will make them much more accepting of the handling they must undergo at the hospital. Talk with us about any concerns you may have. Very stressed or nervous dogs can benefit greatly from having a sedative or anti-anxiety medication given at home prior to the appointment. Let us know if this is something you think your pet would benefit from. Also let us know what worked or didn’t work at the last appointment: Does he/she do better if the exam is done with them on the floor? Does a non-slip mat help? Does your pet do better if he/she waits in the car until we are ready? Our goal as always is to provide the best care possible this includes providing you and your pet as stress-free visit as possible. For more information visit the Fear Free website. by Dr. S. Dawn Dinger, DVM  Vaccinations are one of the best ways to help keep your pet healthy and living a long and happy life. There are many different vaccines that protect against a multitude of different diseases which can affect both your pet and you. Recently though there have been some questions about how often to vaccinate and even what vaccines to give. In part I of this this blog, we'll answer some of the common questions about vaccinations. In parts II and III we'll cover the most current vaccine recommendations for both dogs and cats and talk about what diseases they protect against.  What is a vaccine? Vaccines are substances given to stimulate the immune system. They are usually given by injection, but there are some oral (by mouth) and intranasal (by nostril) vaccines as well. Vaccines contain “antigens” which are designed to look like the disease they are protecting against and which stimulate the production of “antibodies” - small proteins which fight specific infections. This way, if the dog or cat is ever exposed to the real disease, their body is already prepared to fight off the infection. I've heard about core and non-core vaccines. What does that mean? These are terms used by the latest American Animal Hospital Association (AAHA) and American Association of Feline Practitioners (AAFP) vaccination guidelines. In general, “core” vaccinations are those that are considered vital for every pet due to how common the disease is, the risk of exposure, the severity of the disease or the risk to people. These include diseases such as Distemper and Parvo virus for dogs; Panleukopenia and Rhinotracheitis for cats; and Rabies for both species. “Non-core” vaccines are ones that your pet may or may not need depending on their lifestyle and risk of exposure. This does not necessarily mean that the diseases are less severe. Non-core vaccines include diseases such as Bordetella (Kennel Cough) and Feline Leukemia. At Green Valley Veterinary Hospital we will discuss vaccinations for your pet at each wellness visit to help determine what is needed to keep your pet safe.  Are any vaccinations required by law? Typically rabies vaccinations are required by law for dogs and cats over 12 weeks of age in the United States, however individual states may have different requirements as to how often those vaccinations need to be given (IE every year vs every 3 years). How often does my puppy or kitten need to be vaccinated and when do we start? Puppies and kittens receive some antibodies from their mother while nursing (assuming she was properly vaccinated herself). These help protect them from disease while they are very young, however the strength of those antibodies wanes with time. To compensate for this and the fact that young animal's immune systems are still maturing, vaccinations are typically started around 6-8 weeks of age and are continued every 3-4 weeks until they are 16-20 weeks of age. What about my adult dog or cat? The vaccination schedule for adult animals depends on the type of vaccine given, the disease we are protecting against, your pet's overall health and previous vaccination history. Some vaccines may need to be given annually, while others might only need to be given every three years. We will work with you to determine the best vaccination schedule for your pet. Are there any risks? Countless animals have been saved by vaccination so the benefits definitely outweigh the risks. However as with any medical procedure, there is always a small chance of side effects. With the vaccinations available today however, in most cases these risks are quite small compared to the disease itself.  What signs should I watch for? Vaccines stimulate the immune system. It is not uncommon for there to be some mild soreness at the site where the vaccine was given (just like us when we get a vaccine), but a low grade fever or even allergic reactions can develop less commonly. Some signs that warrant veterinary attention include: severe lethargy, vomiting, diarrhea, facial swelling, hives, pallor (looking pale in hairless areas or gums) and collapse. What are Vaccine Associated Sarcomas in cats? A sarcoma is a type of cancer. Most sarcomas that occur are not related to vaccines at all, but some tumors have occurred at the site of vaccinations with Rabies and Feline Leukemia being the most commonly implicated. Most veterinary scientists believe the culprit is the “adjuvant” in those vaccinations (an adjuvant is a substance that is added to some vaccines to stimulate a stronger immune response and prolong the vaccine's action) and so current recommendations are to only administer “non-adjuvanted” vaccines to cats. Rest assured that at Green Valley Veterinary Hospital we only administer the safest vaccinations available to our feline patients. Fortunately vaccine associated sarcomas are quite rare, only occurring between 1 in 1000 to 1 in 10,000 vaccinations. Can I buy and administer vaccinations at home for my pet? The short answer to this question is yes (except for Rabies which by law has to be administered by a licensed veterinarian), but it is not recommended for several reasons. One, vaccines need to be shipped and stored at the proper temperature to maintain their sterility and effectiveness. This can not be guaranteed when purchasing vaccines at the pet or feed store for example. Also vaccinations need to be administered appropriately and in the locations recommended in the current guidelines which can sometimes be difficult without appropriate training and restraint. In addition, syringes and needles are considered medical waste and can not be legally disposed of in the regular trash, and in the event that your pet does develop a problem secondary to the vaccination, you may not be quipped to manage it. Most importantly though is the fact that there is much more to your pet's annual visit that just “shots”. A complete, comprehensive physical exam is the most important part of your pet's visit to the veterinarian, but that visit also includes assessment of and recommedations on things like behavior, diet, parasite control and diagnostic testing, as well as an assessment of risk so the correct vaccinations themselves can be selected. In Part II of this blog, we will discuss the current canine vaccination guidelines and the various disease we are trying to prevent so stay tuned…. by Dr. S. Dawn Dinger, DVM  The holidays are a joyous and fun-filled time for everyone, but they are also a time when inquisitive pets can get themselves into trouble. Here are some tips to keep your pets safe and your holidays happy: 1) Be careful with fireplaces and lit candles - cats especially can burn themselves and have also been known to knock candles over and start fires. 2) Keep the potpourri out of reach. It smells great, but as odd as it sounds, pets will often lick or ingest this. Liquid potpourri especially leads to severe oral ulceration when ingested; dry potpourri less so, but it can lead to an intestinal obstruction if enough is swallowed.  3) All of those holiday goodies can put a strain on our waistline, but they can potentially land your pet in the hospital if ingested. Remember to keep things like chocolate, fatty foods, bread dough, macadamia nuts, onions, grapes, raisins, coffee and alcohol out of your pets reach. 4) Make certain that the Christmas tree has a wide, sturdy base to sit in and you may also want to consider securing it to the ceiling or to a drapery rod, especially if you have large dogs or a cat who may decide that the best view of the tree is from the top! If you have a live tree, keep your pet out of the tree’s water which can contain fertilizers, insecticides and bacteria. Keep lights and electric cords taped to the floor to help keep pets from becoming entangled and to prevent chewing on the wires. Use caution with tinsel as many cats find chewing on this great fun and it can lead to intestinal obstruction if ingested. Keep breakable ornaments securely fastened to the branches and forget about using real popcorn, cranberries or gingerbread garland – even the most well behaved dog will not be able to resist these tasty treats hanging at nose level! 5) Many of the plants and flowers that we use to help decorate our homes can be potentially toxic. Most people have heard that Poinsettias are toxic, but in reality ingestion usually only leads to some GI upset. Holly also will lead to GI distress if ingested. Mistletoe can be more severe and lead to heart problems, but typically this also causes vomiting and diarrhea. A bigger danger are lilies which may be found in Christmas bouquets and arrangements; lilies lead to kidney failure in cats and should not be kept in any room that a cat has access to. 6) Make certain to remind your guests to not sneak snacks to Fido or Fluffy. No matter how cute they are when they beg! (see right) For children it is important to explain the need to respect your pet's wishes if they want a little “alone time”. Also make certain that guests keep any medications, even over-the-counter ones, secured tightly out of pets reach. 7) Use caution with ribbons and bows as these can lead to an intestinal obstruction if ingested, which cats especially are inclined to chew. Keep toys picked up to prevent chewing. Keep an eye on batteries as well – these are very corrosive and can lead to severe burns if bitten or ingested. 8) Be careful with snow globes. Many snow globes contain antifreeze to prevent them from freezing during shipping. Antifreeze (ethylene glycol) is a severe toxin which leads to kidney failure and unfortunately, often death in pets. If a snow globe breaks, keep pets well away from the area until it is thoroughly cleaned as only a few licks of antifreeze can be potentially lethal. 9) Happy Holidays to You and Yours from all of us at Green Valley Veterinary Hospital! by Dr. S. Dawn Dinger, DVM  Autumn brings cool air, blowing leaves, apple cider and, of course, Halloween and plenty of tricks and treats. Most people know that the candy that we give out every year to trick-or-treaters should be kept away from pets, but how much do you really know about the problems that chocolate can cause? As everyone who has one knows, dogs are famous for eating things they shouldn't. Most love food and their keen sense of smell allows them to find even the smallest amounts of food that are hidden away. These traits can prove dangerous however when there is chocolate within Fido's reach.  Chocolate is toxic because it contains “theobromine,” a stimulant similar to caffeine. People are able to metabolize this much better than dogs so it rarely, if ever, causes a problem in humans, but our canine friends are not so lucky. Cats are also not able to metabolize this substance well, but fortunately they rarely have much of a “sweet tooth” so we only occasionally see cats with this poisoning. Symptoms of chocolate toxicity can include vomiting, diarrhea, increased drinking and urinating, hyper excitability, elevated body temperature, muscle tremors, heart arrhythmias, seizures, coma and death. It may take several hours after ingestion for clinical signs to develop and multiple days for signs to resolve even with treatment. Even amounts below toxic doses can lead to GI upset and all the fat and sugar in chocolate can lead to potentially severe problems like pancreatitis, so the safest thing is to avoid having chocolate around dogs at all. The type of chocolate, the amount ingested and the size of the dog, all play a huge role in how toxic it is and what symptoms can be seen. In general, the stronger the chocolate the less that needs to be ingested to cause a problem. White and milk chocolate contain less theobromine per ounce than semi-sweet or baker's chocolate, so a dog would need to eat a lot less of baker's chocolate than milk chocolate to become poisoned. Some general guidelines are that about 1 ounce per pound of body weight of milk chocolate is a dangerous amount, while 0.3 ounce per pound of semi-sweet or 0.1 ounce per pound of baker's chocolate are enough to lead to big problems. So for example, a 10 pound dog could potentially die by ingesting as little as 1 ounce of baker's chocolate; 5 ounces of baker's chocolate could kill a 50 pound dog. Remember these are “lethal” doses; amounts a lot lower than this can still lead to severe problems and some dogs are naturally more sensitive to the effects than others.  So what do you do if your dog ingests chocolate? First, don't panic. Try and determine about how much your dog ate and the type of chocolate and then give us a call (or a veterinary emergency room if we are not available). Depending on this information and the size and overall health of your dog, it may be recommended to bring your dog in for evaluation, to induce vomiting at home or even just to monitor your pet for problems. If you do need to have your pet seen, remember that the sooner you can have them evaluated the better. There is no antidote for chocolate ingestion. Treatment involves limiting absorption by inducing vomiting and giving absorbents and cathartics; helping to flush the system and prevent reabsorption by giving IV fluids; and aggressively treating any signs that develop with things like sedation, oxygen, medications to control heart rate and arrhythmias, and seizure control. Fortunately the prognosis for chocolate toxicity is usually good with rapid and aggressive care. So this Halloween make certain to stay safe and keep all the goodies well out of reach of your pets! Also, as an added tip, avoid using Cocoa Shell Mulch in your garden and flower beds next year – dogs love the taste and ingestion of this can lead to chocolate toxicity too! by Dr. S. Dawn Dinger, DVM  Have you ever wondered how veterinary medicine got started or what your vet needed to do to get where they are now? Here are some fun facts about veterinary medicine that you may not know. 1. References to veterinary medicine have been around for centuries. In fact, the first person credited with being an “expert in healing animals” was a man called Urlugaledinna in Mesopotamia in 3000 BC. The first veterinary school opened in 1761 in Lyon, France. In 1806, Dr. Benjamin Rush (one of our Founding Fathers and a signer of the Declaration of Independence) started lectures at the University of Pennsylvania on “studying the diseases of domestic animals”. In 1879, Iowa State University established the first public veterinary medical school in the United States. 2. Today, there are 30 veterinary colleges in the United States (in contrast to over 170 human medical and osteopathic schools). There are also 5 veterinary colleges in Canada and another 14 internationally which are accredited by the American Veterinary Medical Association, meaning that they pass a rigorous review of their facilities and standards of education. 3. The process of getting accepted into veterinary school is challenging and competitive. Students interested in applying to veterinary school are required to enroll in vigorous pre veterinary curriculums which are heavy in classes such as biology, chemistry, physics and math. Each veterinary school has their own requirements as to what courses are needed, but most prospective veterinary students have a Bachelor's degree at least prior to applying to vet school. Applicants are also required to have extensive animal and veterinary experience as well. Despite this, there are still many more applicants every year than there are spots available.  4. Veterinary school itself is a four year degree program. Its curriculum mirrors that of our human medical colleagues but involves studying a wide range of species, not just one. The first two years are dedicated to studying the normal anatomy and physiology of animals and how the body responds during various disease states. Courses are taken in such things as anatomy, physiology, pharmacology, immunology, pathology and toxicology. The final 2 years have a more clinical focus and include learning about specific diseases and surgical techniques and seeing actual patients under the supervision of veterinarians. 5. For years, veterinary school classes where composed mostly of men however this has changed dramatically over the past 40 years. In 1970, women composed about 10% of the average veterinary class. Today, classes are made up of about 80% women. The career paths of the students have changed as well. In years past, large animal medicine was the career choice for most students (that is, practice focusing mostly on animals such as horses, cows, pigs and sheep). Today, many people still pursue a large animal focus, but the majority of students now plan to enter small animal practice to work mainly on dogs and cats. 6. Have you ever wondered what the difference is between the VMD after Dr. McElhinney's and Dr. Burton-Hall's names and the DVM after Dr. Dinger's? In a nutshell, nothing. Dr. McElhinney and Dr. Burton-Hall received their “Veterinariae Medicinae Doctoris” degree from The University of Pennsylvania, while Dr. Dinger received her “Doctor of Veterinary Medicine” degree from Purdue University. Penn is the only school in the country to confer a VMD degree; the other 29 schools in the US and the 5 in Canada grant DVMs. 7. After graduation, most newly minted veterinarians go into private practice and work on dogs and cats or horses, cows, pigs and other farm animals. Some veterinarians go into exotic animal practice to care for animals such as birds and reptiles. Still others work in animal shelters or zoos. More and more veterinarians are choosing to continue their education another 3-4 years and specialize in one specific area of veterinary medicine such as cardiology, dermatology, ophthalmology or surgery. There are many veterinarians employed in more non-traditional jobs that do not involve direct care of patients. These vets may work in the drug and pet food industries or they may work for the government in the CDC, FDA, NIH and USDA and are involved in biosecurity, public health, disease outbreak investigations and homeland security. There are also a number of veterinarians proudly serving in our military ensuring food safety and caring for military dogs and horses.  8. As in human medicine, veterinary medicine is constantly changing so graduation from veterinary school does not end a veterinarian's education. While formal classroom instruction is over, nearly every state in the country requires a certain number of continuing education hours every year or two years to maintain an active license to practice (Pennsylvania requires 30 hours every two years). This is meant to ensure that your veterinarian is staying current on the latest recommendations and techniques to help your pet. 9. How about veterinary technicians? Technicians also must attend an accredited program (not those correspondence courses that you see on TV!), but there are no pre-veterinary requirements as there are for veterinarians. Most programs are for two years and grant an Associates degree, but there are a few 4 year programs that lead to a Bachelor's degree. Technicians must also pass a credentialing exam and then, depending on the state, are considered either licensed veterinary technicians, registered veterinary technicians or certified veterinary technicians (LVT, RVT or CVT respectively). As with veterinarians, most technicians are employed in private practice, working directly with veterinarians to care for your pet, however technicians can also work in government, industry and the military and some technicians also specialize in specific areas of veterinary medicine such as anesthesia, dentistry, surgery and critical care. 10. You may have noticed on our sign that we are an “AAHA Accredited Hospital”. That sounds good, but what does it really mean? Accreditation is a process by which a hospital's performance and practices are reviewed and compared against current “gold standards” and by which goals are set to continually improve. Unlike in human medicine, veterinary clinics and hospitals are not required to be inspected or accredited, so this is an entirely voluntary process. In fact, only about 15% of veterinary hospitals in the United States have been accredited by the American Animal Hospital Association (AAHA). To become accredited, Green Valley Veterinary Hospital was evaluated on about 900 different standards covering things like patient care, pain management, dentistry, radiology, surgery, emergency procedures and continuing education (all staff, not just the veterinarians are required to complete multiple hours of education every year, far above the amount that is required to maintain a license). To stay accredited, an on-site evaluation is required every 3 years. So, in short, being AAHA Accredited means that we hold ourselves to a very high standard of excellence and that your pet is receiving the highest quality of care that we can provide. by Dr. S. Dawn Dinger, DVM  Have you ever heard of xylitol? Sounds exotic, but chances are you have some in your home right now and it is truly a danger hiding in plain sight for your dog. Xylitol (pronounced zi-li-tol) is a natural sugar substitute and can be found in many sugar free food items such as gum, but as it also has natural anti-cavity effects, it can also found in some toothpastes and mouthwashes. In fact, more and more food items and personal care products, including some peanut butters, ice creams, candies, energy drinks and medications, contain xylitol. Click here for an extensive list of products.  Despite all of it's perks for use in people, xylitol is highly toxic to dogs. Dogs need to ingest much smaller amounts of xylitol than chocolate to be become poisoned and many pet owners are unaware of the dangers, so cases of poisonings are becoming more and more frequent. Unlike in people, xylitol stimulates the release of insulin in dogs which can lead to life threatening hypoglycemia (low blood sugar). Signs of hypoglycemia in dogs can include weakness, seizures and coma and can develop in as little as 30 minutes after ingestion, but can be delayed out to about 18 hours if the xylitol is contained in a substance which will slow it's absorption (like gum). However, the problems don't end there. Several days after ingestion of xylitol, some dogs will develop acute liver failure. Many of the dogs that develop liver failure did not develop low blood sugar after the initial ingestion. At this time, it is not known why that occurs. So how much is too much? Dogs need to ingest about 0.1 gr/kg (gram/kilogram) of xylitol to develop hypoglycemia and about 0.5 gr/kg to develop liver failure. So a 20 pound dog would need to ingest 0.9 gr to become hypoglycemic and about 4.5 gr to be at risk for liver failure. A sugar packet typically contains about 1 gr of xylitol and a stick of gum typically contains 0.3 – 2 gr of xylitol. So this means that our 20 pound example dog would only need to ingest one or two sticks of gum to be in big trouble. As any dog owner knows, most of our goofy, glutinous canine friends can swallow that in a gulp. What happens then if you come out to the kitchen and find that your dog has gotten into your purse and ingested a pack of sugar free gum? First, call us immediately! If this is at a time we are not in the office, call a veterinary emergency room (See PVSEC's information at the bottom of our website). Your dog will likely need to be seen right away. Make certain to take the package of food, medication etc with you and try to have an idea of how much your dog ate. Your veterinarian will need to try and calculate the dose of xylitol that you dog ingested. Sometimes that is easier said than done – xylitol may be listed on the ingredient list, but the actual concentration is often considered proprietary information and can be difficult to obtain. Your vet may need to go on the “most likely” maximum amount ingested based on averages that that type of product typically contains.  Depending on when ingestion occurred and how much was ingested, your vet may induce vomiting in your dog to help get rid of as much product as possible. They will also likely need to check labwork, including blood glucose level and liver values. At at minimum your dog may need to be admitted and monitored for some time to make certain no problems develop. If your dog is already hypoglycemic, then they will need to be hospitalized on intravenous (IV) fluids and dextrose (a sugar). Low blood sugar can persist 12 – 48 hours; once your dog is able to maintain his blood glucose within normal range on his own he will be able to go home, but will need monitoring of his blood glucose and liver values over another few days. Luckily the prognosis is good if no signs develop or if the hypoglycemia is treated rapidly. Unfortunately, the same can not be said for those dogs that develop liver failure. Signs of liver failure can include vomiting, diarrhea, dark/tarry stools, jaundice (yellow gums or skin), bleeding, or bruising and typically develop 2-3 days after ingestion. Liver failure is treated aggressively with things like fluids, plasma transfusions, antibiotics and liver protectants, but there is no specific antidote for xylitol toxicity. Sadly, once liver failure develops, the prognosis is poor.  Obviously, the best thing you can do is to prevent exposure in the first place. Never leave purses, bags etc out where curious canines can get into them. Never allow pets to beg or receive food from the table. Be especially careful if anyone at home is a diabetic or if you do any sugar free baking. Make certain to keep all medications out of reach and be careful when walking your dog too – those discarded wads of gum on the sidewalk can be snatched up by your pup very quickly. Don't forget to check the ingredient lists on packages also, especially on anything that you might use to make a treat for your dog. Some “key words” that should put up red flags include: sugar free; reduced sugar; all natural; no artificial sweeteners; birch sugar; safe for diabetics; low carb; low cal; and anti-cavity. And lastly, a word about cats. Does xylitol affect them the way it does dogs? In short, we don't know. According to National Animal Poison Control, to date there have been no reported cases of toxicity developing in cats. Is that because they are more resistant to xylitol's effects, or just because cats are less greedy than dogs and so less likely to ingest things like gum and candies? Again, we don't know, so the safest course of action is to keep your cat away from these products as well.
by Crysta Clear, CVT

Don't let a little bit of rain get in the way of a fun-filled day! We all know that our best friends can get themselves into trouble if they haven't had enough attention or exercise, not to mention the boredom of being stuck inside. Our pups rely on us to stay entertained. While some dogs refuse to get their paws wet, some are ready to make a mess that you may not want to have to clean up! Either way, there are plenty of ways to tire out your pets on a rainy day and avoid the downpour!
1. TEACH YOUR OLD DOG SOME NEW TRICKS:
There is no better activity to exhaust your pooch other than putting on a lesson! There is a never-ending variety of commands that you could teach your dog. You'd be surprised how far a small amount of time and patience can get your dog! And when class is in session, your dog will feel bonded to you by wanting to please you, will be happy with earning treats, and will come out with a new skill. You can search for any trick on Youtube to find a tutorial like the ones below:
2. PLAY OR INVENT YOUR OWN INDOOR GAMES:
Everybody loves Pinterest, right?! Look up "indoor games for dogs" and check out the endless options that people more creative that you or I have come up with! Whichever idea you "borrow", whether it's the homemade toys, obstacle courses, fetching up the stairs, or games like hide and seek, the options are infinite and if Fido doesn't like one, there are more to try! Some of the easiest options can be found in the following video as well:
(via Cone of Shame with Dr. Andy Roark)

3. FOOD-DISPENSING OR PUZZLE TOYS:
Mental stimulation is the best trick if you don't have the time or energy yourself to spend with your dog after you've worked a long day. There are many toys that you can buy at the pet store with varying levels of difficulty, but they can be on the expensive side or require specific sizes or shapes of treats and refills. Some wonderful options are Kong brand toys (e.g. Wobbler food-dispensing toy, Marathon treat-ball, or Pawzzles), the Everlasting Treat Ball, or other available puzzle games. You could also skip all of the cost and hassle and make some yourself!
(via Michelle Huntting)
4. VENTURE OUT OF THE HOUSE ANYWAY:
There are lots of indoor activities that just take a run through the rain to get to the car. You could make a shopping trip to a pet store in the area! There are also many options for Indoor Dog Parks, Playgrounds, Day Care, Boarding, Grooming, and Training facilities in the Pittsburgh area. Check out the list below and click their links for more information:
Animal Friends
Pittsburgh, PA Misty Pines Sewickley, PA Lucky Paws Pet Resort Freedom, PA Camp Bow Wow Pittsburgh, PA (several locations) Get Smart! Training Center (WPA Humane Society) Pittsburgh, PA and Crafton, PA The Dog Stop Wexford, PA
*Disclaimer: GVVH does not endorse any facilities or products listed in this blog post and results may vary. Contact these facilities prior to attending and make sure that your dog is protected and vaccinated according to their requirements. Always supervise your pet with toys.
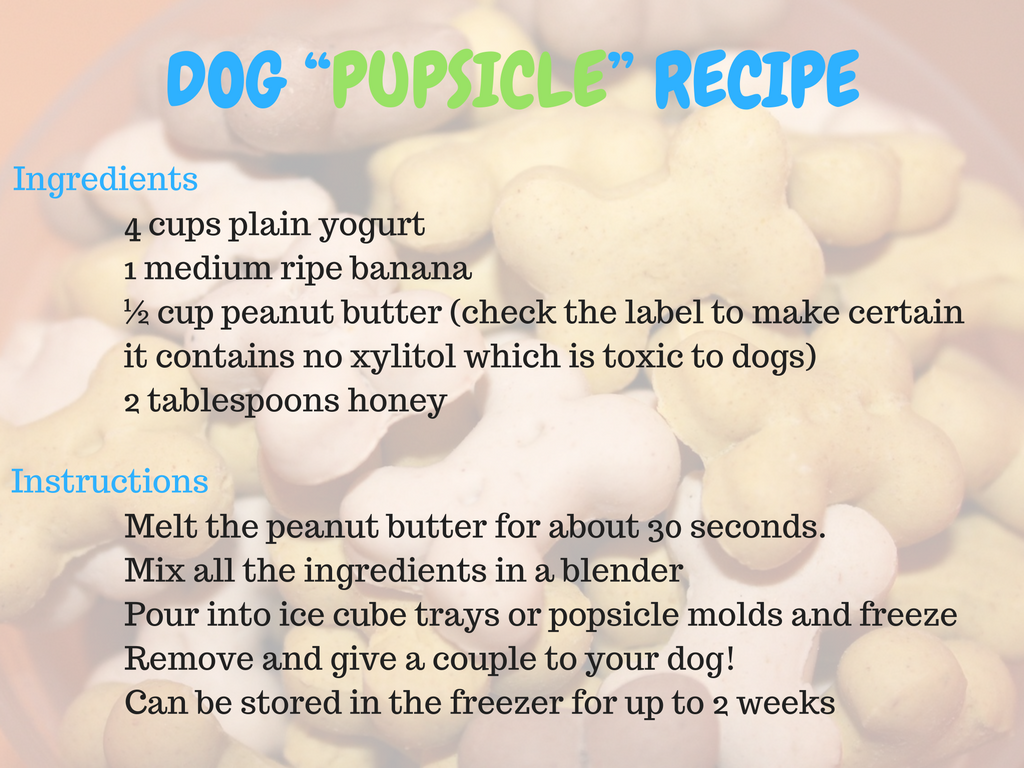
by Dr. S. Dawn Dinger, DVM  The dog days of summer are finally upon us and with it comes baseball, barbecues and a plethora of other outdoor activities. Summer also comes with some hazards too, so here are ten tips to help keep your pets safe this season. 1. NEVER LEAVE PETS IN A CAR: Temperatures inside a vehicle can rise to dangerous levels within a few minutes. Even on a relatively mild 80 °F day, the temperature inside the car will be 114°F within 30 minutes. Heatstroke and subsequent brain damage and death can occur rapidly in these conditions. Never leave your pet in a car unattended even in the shade with the windows down.  2. HAVE PLENTY OF SHADE AND WATER: Pets can also overheat on hot days when left outside. Make certain they always have access to fresh, cool drinking water and plenty of shade. Better yet, keep them inside during the hottest part of the day and keep walks and other activities to a minimum. 3. KNOW THE SIGNS: Symptoms of overheating include heavy panting or difficulty breathing; weakness; drooling; and in severe cases, vomiting, bloody diarrhea, collapse and seizures. Body temperatures are often well over 104°F (normal 100°F - 102.5°F). Some animals are more susceptible to overheating than others – elderly pets, those who are overweight or have underlying heart or lung disease are at greater risk. Some breeds are also predisposed: “smushy faced” breeds such as bulldogs, pugs and Persian cats, don't move air as well and can easily overheat. If you have concerns that your pet may be overheating, move them to a cool area, put a fan in front of them and apply cool (not cold) water to their feet, legs and belly. Call us right away for further instructions.  4. BEWARE OF HOT PAVEMENT: We've all seen the videos of eggs frying on the sidewalk. While these are fun to watch, it's a lot less enjoyable when it's your pet's feet! Asphalt temperatures can reach 135°F on an 86°F day and tissue damage can start in as little as 60 seconds. We can see severe burns on animal's feet as a result. Don't walk your pet during the hottest part of the day and avoid asphalt and other hard surfaces, stick to grass or dirt instead. 5. SUNBURNS: Did you know that dogs and cats can get sunburn? They can and this can eventually lead to skin cancer just like in people. While the hair provides some protection from the sun, prolonged exposure can lead to problems. Animals with white or light colored fur and hairless breeds are at especially high risk. Make certain to slather on the a pet sunscreen if your pet will outside for a long period and especially concentrate on areas with thinner hair such as muzzles and bellies. 6. WATER SAFETY: Contrary to what “You Tube” would have you believe, not every pet can swim, or even likes to. Use caution around water and use a specially-made pet life preserver if your pet will be swimming or on a boat. Also, do not allow your pet to ingest a lot of water all at once. Pool water and water from rivers and lakes contain chemicals and bacteria, but “water intoxication” causes severe shifts in electrolytes in the body due to over hydration and can be life threatening. 7. WATCH OUT FOR UNINVITED GUESTS: Fleas, ticks, mosquitoes and other parasites are at their worst this time of year and can make your pet not only miserable, but can spread disease as well. Make certain you are keeping up on your pet's flea, tick and heartworm preventatives. Give us a call if you have any questions and we'll be happy to help you with that. 8. WATCH OUT FOR UNINVITED GUESTS PART 2: Things that sting and bite are also in abundance. Bees, hornets and wasps are everywhere and can easily be stepped on. Some dogs and cats also enjoy chasing and biting these flying hazards. If your pet is stung and seems painful or develops any hives, facial swelling or vomiting, they should be evaluated by a veterinarian right away. Snakes are also easily found both in parks and on hikes, but also in your own backyard. Dogs especially are often bitten on the legs, chest and face. Snakes bites can be potentially dangerous and any that occur should be checked out as soon as possible.  9. COOKOUTS: Pets love to take part in any of our activities and if it involves food that's even better! However, be aware that meats and bones can lead to problems like GI upset, pancreatitis and obstructions and therefore should not be given to pets. Be careful to keep the trash covered also, as many pets will rip open bags to get at the contents. Things like corn cobs often get stuck in the intestines and toothpicks and meat skewers can injure the mouth and puncture the esophagus or intestine. 10: VACATION TIME: This is also the time that we travel the most, and many times, take our pets with us. Remember that pets can be easily frightened in new environments and may not behave or respond to commands as they usually do. Make certain they are always properly restrained on a leash or in a carrier and that they wear up to date identification in case the worst happens and they get lost. BONUS: (Please note, if your pet is prone to GI upset or pancreatitis; is a diabetic; is on a hypoallergenic or other prescription diet, please contact us before giving these treats to your pet).
by Crysta Clear, CVT Thanks for visiting our new and improved website! On this new page we plan to post useful information, up to date veterinary recommendations, and real-life stories from our clinic!
You can check this page for new posts or stay tuned in to our blog via our Facebook page where we post a link any time we post a new blog post. If you have any feedback on our website or blog posts, you may leave a comment here or on our Facebook page. If you'd like to write a review of our clinic, please visit our Google page! |
AuthorsDr. S. Dawn Dinger, DVM Archives
May 2017
Categories |
 RSS Feed
RSS Feed